Udaipur, Rajasthan
Earlier this year, in March, 45-year-old Kasna Garasiya, a resident of Kaucha village in Udaipur district, complained of pain in his limbs. His family members rushed him to a local ‘doctor’ — a jhola chhaap (a quack ) — in Kotda town.
“He was put on a drip at the clinic but soon his condition worsened. While we were taking him to a hospital in Udaipur city, he breathed his last on the way,” the deceased’s relative told Gaon Connection.
Quite similar is the story of Bhanwar Lal Meghwal of Manna Ji Ka Guda village in the Gogunda block. His wife, 27-year-old Bhoori Bai, fell sick on September 25, 2019. She was taken to a jhola chhaap who administered an intravenous injection to ‘treat’ her.
“Upon being injected, her condition deteriorated. Then, we took her to Maharana Bhupal Government Hospital in Udaipur but soon after, the doctors declared her dead. I couldn’t believe that my wife was no more!” Bhanwar Lal Meghwal told Gaon Connection.

Rural India is replete with tragic instances of deaths of villagers like Kasna Garasiya and Bhoori Bai, who fail to receive proper treatment through a trained medical professional. A large chunk of rural India population is still dependent on unqualified healthcare providers popularly known as jhola chhaaps or bangaali daaktar.
Rural India has a severe shortage of human resources for health, commonly referred to as HRH. India is one of the 57 countries with a critical HRH shortage, as noted in a January 2022 paper titled, ‘Workforce problems at rural public health-centres in India: a WISN retrospective analysis and national-level modelling study’.
As per this research study, the national density of doctors, nurses, and midwives was found to be 20.6 per 10 000 people compared to the World Health Organization (WHO) recommendation of 44.5. Also, there are significant urban–rural differences in HRH with urban areas having four times greater doctor density than rural areas.
To enhance health services and improve HRH access in rural India, the Ministry of Health and Family Welfare (MoHFW) launched the National Rural Health Mission (NRHM) in 2005. Despite several years of its implementation, HRH shortage still persists in rural areas. And villagers depend either on jhola chhaap or health workers to meet their medical needs including treatment of diseases.

A large chunk of rural India population is still dependent on unqualified healthcare providers popularly known as jhola chhaaps or bangaali daaktar.
Also Read: Networking for rural healthcare in tribal regions of Tamil Nadu
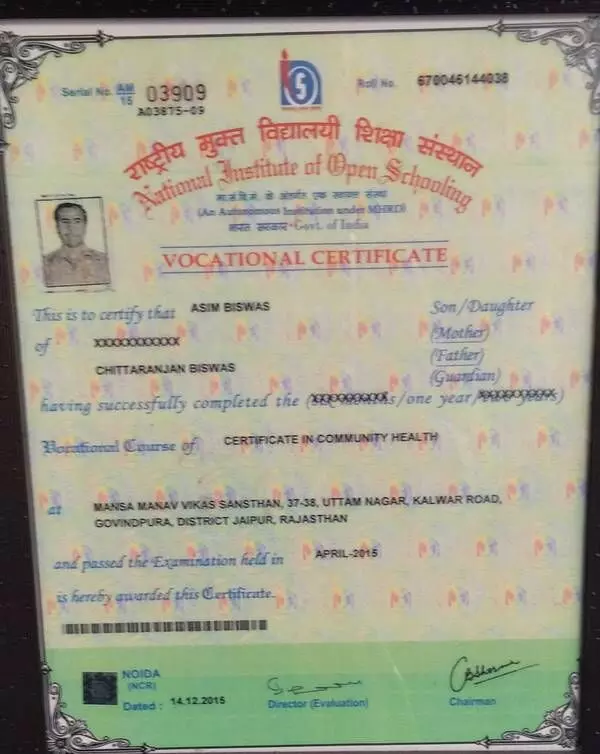
“In India, almost 1,500,000 health workers have the experience of first aid and preventive healthcare but don’t have any certificates so the government began certifying such professionals. However, these people can only provide first aid and refer the patients to higher authorities or institutions. If these people are providing medicines to patients then it’s completely wrong,” Vijay Bhushan, director of Mansa Institute of Medical and Health Sciences, told Gaon Connection.
This Jaipur-based institute is one of the institutes authorised to grant certificates to the health workers, who, Bhushan said, do not have the authority to hand out medicines to the patients.
But, the ground reality is very different.
In the Gogunda town of Rajasthan’s Udaipur district, ‘Priyanto Clinic’ is run by a middle-aged doctor. Adjacent to the ‘doctor’s’ table is a green curtain behind which are small beds that are used to administer injections and drips to the patients.
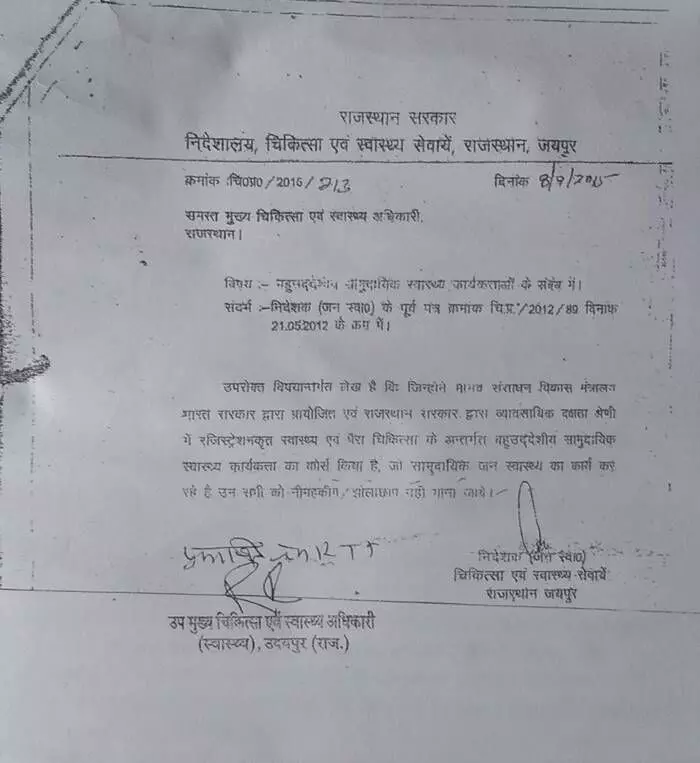
Investigations against these fraud doctors were inconclusive because of this government order dated September 8, 2015.
Also Read: “I may be a jhola chaap, but I help villagers in their times of distress”
In October 2019, in an investigation led by the Udaipur-based OP Raipuriya, the then block chief medical and health officer [BCMHO] in the Department of Medical, Health and Family Welfare, the ‘doctor’ who runs this clinic was found to have attended the school till class 10th.
However, on being questioned, the ‘doctor’ told Gaon Connection that he had studied a course named ‘B-S-A-M’ but couldn’t answer what the abbreviation stood for.
Meanwhile, Raipuriya, the officer who led the inquiry against the ‘doctor’ lamented that most of the investigations against these fraud doctors were inconclusive because of a government order dated September 8, 2015.
“When we raid such clinics in the rural areas, the incharge doctors show us a certificate of being a health worker which is issued by the Community Health Centres. The state government has mentioned in a notice that such workers should not be clubbed as neem hakeem [traditional medicine practitioners] or jholachhaaps,” Raipuriya said. “What should be done to keep them from providing treatment which they are not authorised to, is not mentioned in the government order,” he added.
When Gaon Connection accessed one such certificate from a jhola chhaap doctor in Udaipur, it was learnt that these health workers are certified to provide preventive healthcare, oversee child and maternal health and provide first aid during emergencies in areas that do not have sufficient formal medical staff available.
Despite the inquiry against him by Rajasthan’s health department in 2019, the ‘doctor’ at ‘Priyanto Clinic’ continues to run his clinic with patients queuing at his health facility.
Narendra Gupta, a Chittorgarh-based medical practitioner and member of the Prayas NGO told Gaon Connection that despite the lethal risks involved in the functioning of these unauthorised healthcare providers, their role has become almost indispensable especially in the rural and the tribal regions where government’s healthcare facilities are virtually non-existent.
“In Rajasthan, there are as many jhola chhaaps as there are villages in the state. Many patients lose their lives too. The relatives don’t complain because this is the only form of healthcare available to them for twenty four hours a day. Most of the jhola chhaaps are respected by the rural folks for the work they do,” he said.
Note: This story was reported under NFI Fellowships for independent journalists.




















